EXHIBIT 99.2
Published on November 14, 2023
|
INNOVATING FOR PATIENTS Nasdaq TRVN I November 2023 |
|
Forward-Looking Statements To the extent that statements contained in this presentation are not descriptions of historical facts regarding Trevena, Inc. (the “Company” or “we”), they are forward-looking statements reflecting management’s current beliefs and expectations. Forward-looking statements are subject to known and unknown risks, uncertainties, and other factors that may cause our or our industry’s actual results, levels of activity, performance, or achievements to be materially different from those anticipated by such statements. You can identify forward-looking statements by terminology such as “anticipate,” “believe,” “estimate,” “expect,” “intend,” “may,” “might,” “plan,” “objective,” “predict,” “project,” “suggest,” “target,” “potential,” “will,” “would,” “could,” “should,” “continue,” “ongoing,” or the negative of these terms or similar expressions. Forward-looking statements contained in this presentation include, but are not limited to, (i) statements regarding the timing of anticipated clinical trials for our product candidates; (ii) the timing of receipt of clinical data for our product candidates; (iii) our expectations regarding the potential safety, efficacy, or clinical utility of our product candidates; (iv) the size of patient populations targeted by our product candidates and market adoption of our potential drugs by physicians and patients; (v) the timing or likelihood of regulatory filings and approvals; and (vi) our cash needs. Actual results may differ materially from those indicated by such forward-looking statements as a result of various important factors, including: the commercialization of any approved drug product, the status, timing, costs, results and interpretation of our clinical trials or any future trials of any of our investigational drug candidates; the uncertainties inherent in conducting clinical trials; expectations for regulatory interactions, submissions and approvals, including our assessment of the discussions with the FDA or other regulatory agencies about any and all of our programs; uncertainties related to the commercialization of OLINVYK; available funding; uncertainties related to our intellectual property; other matters that could affect the availability or commercial potential of our therapeutic candidates; and other factors discussed in the Risk Factors set forth in our Annual Report on Form 10-K and Quarterly Reports on Form 10-Q filed with the Securities and Exchange Commission (SEC) and in other filings we make with the SEC from time to time. In addition, the forward-looking statements included in this presentation represent our views only as of the date hereof. We anticipate that subsequent events and developments may cause our views to change. However, while we may elect to update these forward-looking statements at some point in the future, we specifically disclaim any obligation to do so, except as may be required by law. 2 |
|
Trevena Overview 3 Focused on Innovative Medicines For CNS Disorders Olinvyk IV* Approved NCE for the management of acute pain in adults* Proven track record of Trevena internal discovery and development through approval S1P Modulator Program Novel S1P1R modulator with differentiated MOA (lead asset: TRV045) Preliminary data from proof-of-concept studies for CNS disorders Innovative CNS Pipeline Based on Nobel-prize winning biased ligand technology NCEs addressing acute / neuropathic pain, epilepsy, acute migraine, OUD1 Detailed in Following Slides * OLINVYK is indicated in adults for the management of acute pain severe enough to require an intravenous opioid analgesic and for whom alternative treatments are inadequate. Please see Important Safety Information including BOXED WARNING at the end of presentation. Full Prescribing Information at www.OLINVYK.com. 1 OUD = opioid use disorder |
|
TRV045: Innovative Clinical-Stage S1P1R Modulator TRV045: Selective S1PR Modulator Compelling Clinical POC Data1 Differentiated Product Profile Large Addressable Target Indications Novel Family of S1PR Modulators S1PR: Validated target for multiple blockbusters (fingolimod / siponimod / ozanimod / ponesimod) TRV045: Unique profile with no lymphopenia or cardiac / ophthalmologic / pulmonary AEs Statistically significant, dose-dependent effect in validated model of neuropathic pain Statistically significant EEG changes and evidence of early reduction in cortical excitability Novel MOA; expected once daily oral dosing; potentially effective with favorable safety/tolerability Potential for favorable cognitive profile vs current SOC Initial investigation for orphan / non-orphan non-opioid chronic pain and epilepsy Broad potential application in CNS disorders, autoimmune disease and inflammatory disease New chemical entity; potent and selective for subtype 1; developed in-house with strong IP NIH collaboration: Epilepsy Therapy Screening Program & Preclinical Screening Pain Platform 4 SOC = Standard of Care MOA = Mechanism of action 1Studies were conducted outside the United States and not under the IND for TRV045 |
|
S1P1 Receptor – Novel Target for CNS Indications 1) Sim-Selley et al., Journal of Pharmacology & Experimental Therapeutics, 2018. 2) Sim-Selley et al, Journal of Neurochemistry, 2008. 3) Gol et al., European Journal of Pharmaceutical Sciences, 2017. 4) Leo et al, CNS & Neurological Disorders - Drug Targets, 2017. 5) Choi, et al. PNAS 2011. S1P1 receptors are highly expressed on key CNS cells involved in neuroinflammation Potential therapeutic role in seizures, epileptogenesis and pain signaling Neuropathic pain • Inhibits pain sensation1 • Inhibits excitatory neuronal signaling2 Existing S1PR-targeted drugs, however, are ill-suited for CNS indications due to known: Lymphopenia Pulmonary AEs Cardiac AEs Ophthalmologic AEs Epilepsy • Neuroprotective effects3 • Modulates BBB permeability, anti-inflammatory effects4,5 5 |
|
TRV045 MOA (1): Rapid Receptor Recycling β-arrestin2 S1P1 receptor Gβγ GRK ↑I Internalization KAch ligand Gαi ↓cAMP ↓ Ca++ (via IcaL) Reduces surface receptor, which leads to lymphopenia (Gilenya, etc) Receptor Recycling Maintains surface receptor and avoids lymphopenia, allowing free lymphocyte egress into circulation Receptor Degradation Other S1PR Drugs TRV045 6 Maintained (rather than degraded) S1P receptors on cell surface No lymphopenia reported in prior Phase 1 FIH study Maintained surface receptor, allowing free lymphocyte egress into circulation FIH = First in human Source: Trevena data on file |
|
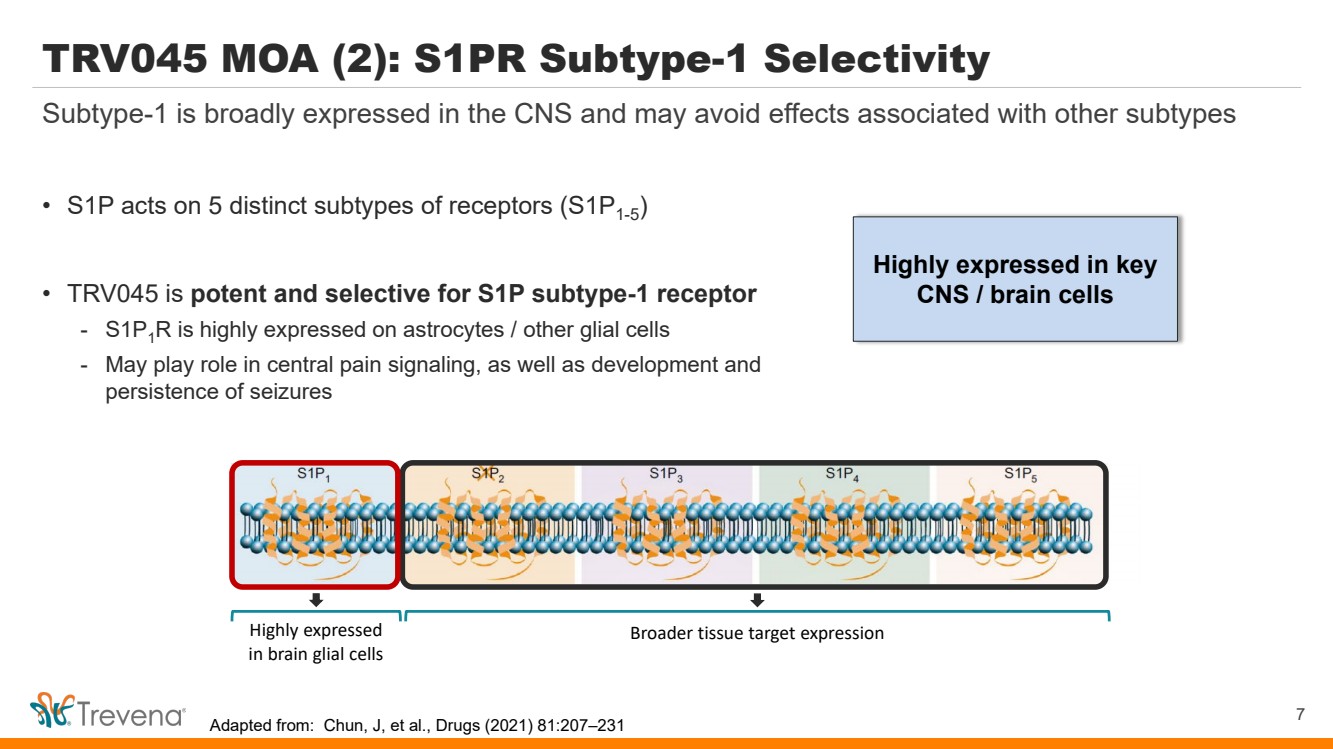
Highly expressed in key CNS / brain cells TRV045 MOA (2): S1PR Subtype-1 Selectivity • S1P acts on 5 distinct subtypes of receptors (S1P1-5) • TRV045 is potent and selective for S1P subtype-1 receptor - S1P1R is highly expressed on astrocytes / other glial cells - May play role in central pain signaling, as well as development and persistence of seizures 7 Subtype-1 is broadly expressed in the CNS and may avoid effects associated with other subtypes Highly expressed in brain glial cells Broader tissue target expression Adapted from: Chun, J, et al., Drugs (2021) 81:207–231 |
|
1) P<0.05 v vehicle 2) Full cytokine / chemokine panel studied: (Inflammatory markers) – TNFa, IL-6, IL-1b, IL-17, IL-23, IL-33, CCL1, CCL2, CCL20, CXCL5, CXCL12, CX3CL1, IFNg, Csf2, Substance P; (Anti-inflammatory markers) – IL-10, IL-4. (Trevena, Inc., data on file) TRV045 MOA (3): Anti-Inflammatory Effect (nonclinical) • Main Findings: Net anti-inflammatory action (statistically significant) on astrocyte cytokine / chemokine release - Increased all anti-inflammatory markers measured1 - Reduced all inflammatory markers measured1 • Method: Primary mouse astrocytes in monolayer cell culture, incubated for 24hrs w/ 5 µM TRV045 - 17 cytokines / chemokines2 assessed by ELISA TRV045-affected cytokines / chemokines play a role in many CNS disorders (epilepsy, pain, neuropsych / neurodegen diseases) Anti-inflammatory actions (cytokines / chemokines) on astrocytes in cell culture 8 -150 -100 -50 0 50 100 150 IL-1b TNFa IL-17 CXCL5 IL-4 IL-10 % Change from Vehicle Anti-markers inflammatory Inflammatory markers |
|
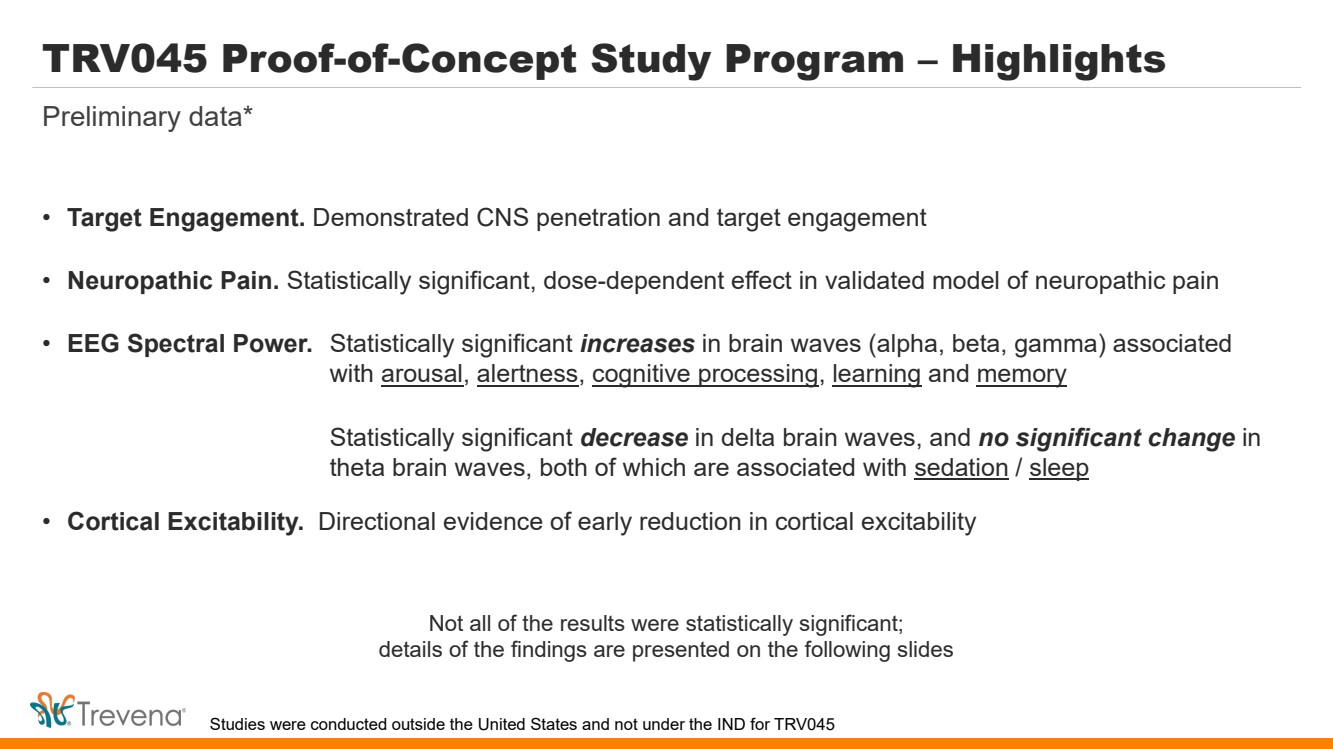
TRV045 Proof-of-Concept Study Program – Highlights • Target Engagement. Demonstrated CNS penetration and target engagement • Neuropathic Pain. Statistically significant, dose-dependent effect in validated model of neuropathic pain • EEG Spectral Power. Statistically significant increases in brain waves (alpha, beta, gamma) associated with arousal, alertness, cognitive processing, learning and memory Statistically significant decrease in delta brain waves, and no significant change in theta brain waves, both of which are associated with sedation / sleep • Cortical Excitability. Directional evidence of early reduction in cortical excitability Preliminary data* Not all of the results were statistically significant; details of the findings are presented on the following slides Studies were conducted outside the United States and not under the IND for TRV045 |
|
TRV045 POC Study Program – Overall Objectives • Provide evidence of CNS penetration and target engagement via pharmacodynamic effects on validated experimental study endpoints in humans, using: - Battery of acute and chronic pain models (characterize ‘analgesic phenotype’ for TRV045) - EEG and EMG measures of changes in resting state brain electrical activity on and off drug and TMS-stimulated brain cortical excitability • Provide PK-PD exposure data to guide future formulation development efforts and dose range selection for future Phase 2 studies - Prior phase 1 data demonstrated PK profile consistent with anticipated once-daily dosing • Provide additional safety and tolerability data to support results of initial Phase 1 FIH study - No lymphopenia - No cardiovascular signals of concern - No evidence of ophthalmologic, pulmonary adverse effects 10 Preliminary data* * Complete safety and tolerability data expected early 4Q 2023 Studies were conducted outside the United States and not under the IND for TRV045 Source: Trevena data on file |
|
Target Engagement (PainCart®) POC Study Design • Pharmacodynamic Endpoints: - Mechanical allodynia (Von Frey hair testing on capsaicin-treated skin), pressure pain, heat pain (capsaicin-treated, UVB-exposed, and unexposed skin), cold pain (CPT), electrical pain (stair, burst conditions), conditioned pain modulation (electrical pain pre- and post-CPT) • PK exposure parameters (Cmax, t½) • Safety and tolerability 11 • Design: Randomized, double-blind, placebo-controlled, single dose, four-way cross-over (N=25 subjects; 8F/17M, mean age 37.6 years, range 18-53) - Placebo or TRV045 (50/150/300mg) Studies were conducted outside the United States and not under the IND for TRV045 Source: Trevena data on file |
|
TRV045 Significantly Reduced Mechanical Allodynia 12 1% capsaicin-treated dominant volar forearm – Von Frey filament allodynic area (CFB, mm2) Change from Baseline (mm2) -1200 -1000 -800 -600 -400 -200 0 200 400 600 Baseline Hr 1 Hr 2 Hr 4 Hr 6 Hr 8 Hr 10 Total Allodynic Area Placebo 50mg 150mg 300mg -1200 -1000 -800 -600 -400 -200 0 200 400 600 Baseline Hr 1 Hr 2 Hr 4 Hr 6 Hr 8 Hr 10 Secondary Allodynic Area Placebo 50mg 150mg 300mg 300mg TRV045 v Placebo; P=0.0023 150mg TRV045 v Placebo; P=0.0022 300mg TRV045 v Placebo; P=0.0001 150mg TRV045 v Placebo; P=0.0002 Source: Trevena data on file |
|
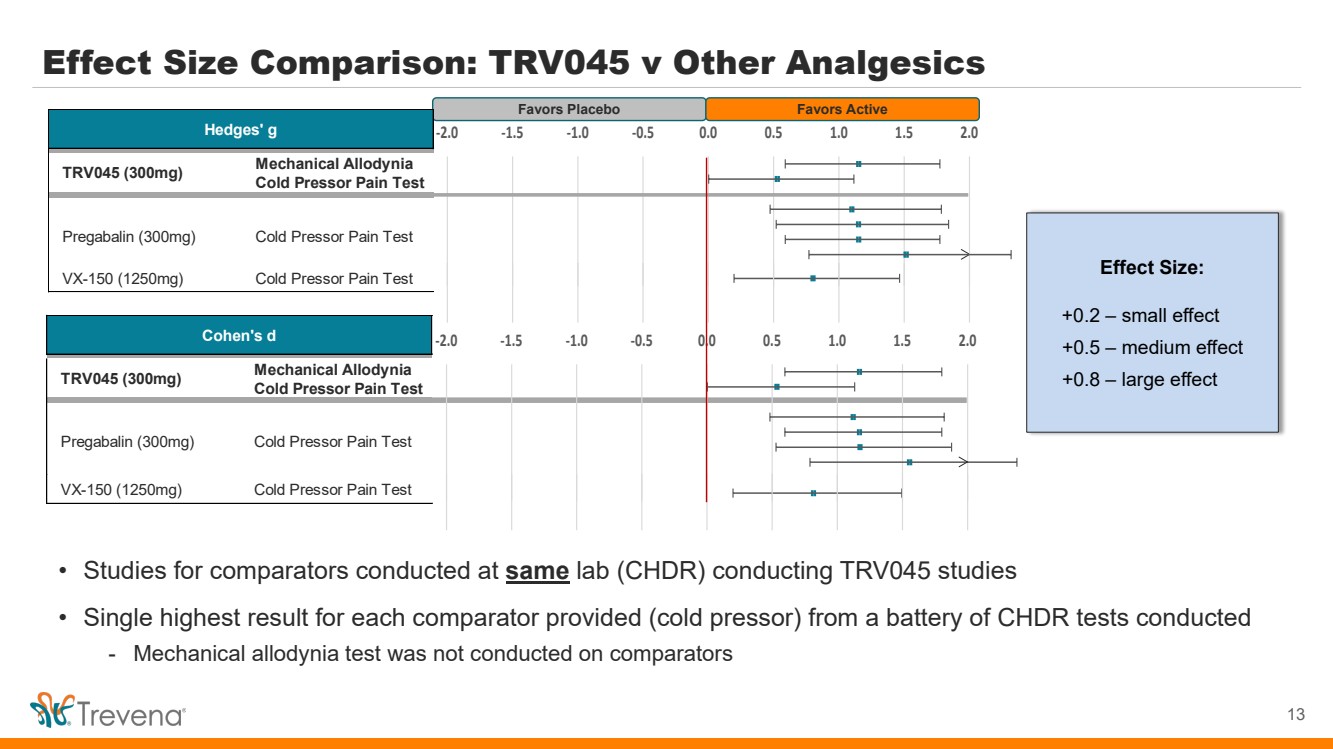
Effect Size Comparison: TRV045 v Other Analgesics 13 Favors Placebo Favors Active • Studies for comparators conducted at same lab (CHDR) conducting TRV045 studies • Single highest result for each comparator provided (cold pressor) from a battery of CHDR tests conducted - Mechanical allodynia test was not conducted on comparators Effect Size: +0.2 – small effect +0.5 – medium effect +0.8 – large effect VX-150 (1250mg) Cold Pressor Pain Test Mechanical Allodynia Cold Pressor Pain Test Hedges' g Cold Pressor Pain Test TRV045 (300mg) Pregabalin (300mg) -2.0 -1.5 -1.0 -0.5 0.0 0.5 1.0 1.5 2.0 VX-150 (1250mg) Cold Pressor Pain Test Mechanical Allodynia Cold Pressor Pain Test Cohen's d Cold Pressor Pain Test TRV045 (300mg) Pregabalin (300mg) -2.0 -1.5 -1.0 -0.5 0.0 0.5 1.0 1.5 2.0 |
|
Source: Trevena data on file Target Engagement (PainCart®) Study • Statistically significant, dose-dependent, treatment effect in model of capsaicin-induced mechanical allodynia provides evidence of the therapeutic potential of TRV045 in neuropathic pain - Recognized and validated study index of central pain processing (‘central sensitization’) - Note that effect appeared similar with both 150mg and 300mg dose, potentially guiding future decisions on dose range for use in Phase 2 • Supportive evidence of analgesic action in select other nociceptive models - Other endpoints did not show trend / statistically significant results (pressure pain / conditioned pain modulation) • Overall, strong support for CNS penetrance and engagement of pain signaling pathways in the brain - PK exposure consistent with parameters observed at comparable doses studied under fed conditions in Phase 1 FIH study • No SAEs, no drug-related study discontinuations 14 PainCart observations |
|
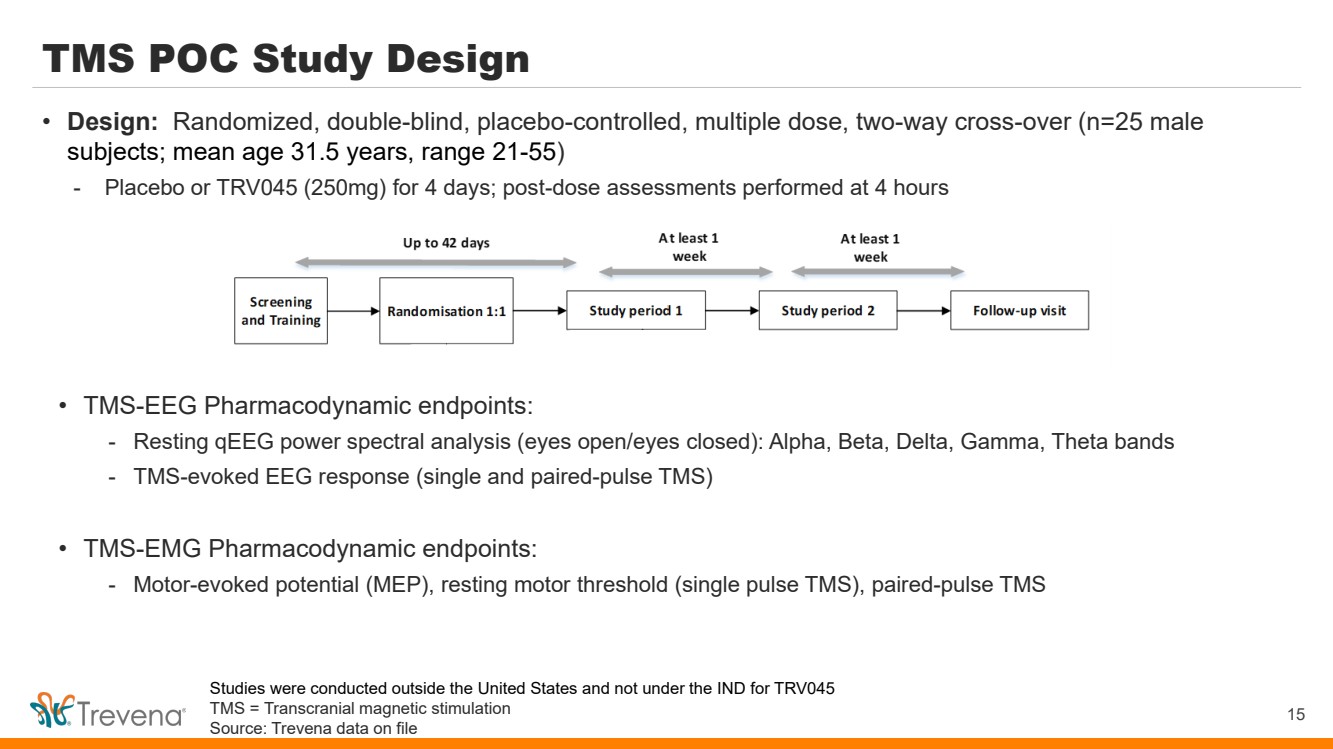
TMS POC Study Design • TMS-EEG Pharmacodynamic endpoints: - Resting qEEG power spectral analysis (eyes open/eyes closed): Alpha, Beta, Delta, Gamma, Theta bands - TMS-evoked EEG response (single and paired-pulse TMS) • TMS-EMG Pharmacodynamic endpoints: - Motor-evoked potential (MEP), resting motor threshold (single pulse TMS), paired-pulse TMS 15 • Design: Randomized, double-blind, placebo-controlled, multiple dose, two-way cross-over (n=25 male subjects; mean age 31.5 years, range 21-55) - Placebo or TRV045 (250mg) for 4 days; post-dose assessments performed at 4 hours Studies were conducted outside the United States and not under the IND for TRV045 TMS = Transcranial magnetic stimulation Source: Trevena data on file |
|
EEG Shifts in Alpha, Beta, Gamma, Delta Power Spectra -5 0 5 10 Delta Theta Alpha Beta Gamma TRV045 Placebo 16 Resting qEEG Power Spectral Analysis – Eyes Open, Day 4 TRV045 v Placebo All Bands -5 0 5 10 Delta Theta Alpha Beta Gamma TRV045 Placebo -5 0 5 10 Delta Theta Alpha Beta Gamma TRV045 Placebo * * * * * * +21.3% -15.2% +23.1% +40.7% +38.8% +26.6% (µ V 2) CFB (µ V 2) CFB (µ V 2) CFB Frontal* Left Parietal* Right Parietal* Alpha: Significant increase across all regions Beta/Gamma: Significant increase in frontal region Delta: Significant reduction in right parietal region Theta: No significant difference associated with alertness / arousal memory / learning associated with sedation / sleep Mantini, D, et al. PNAS (2007); Beste, C, et al. Nature Comm Biol (2023); Edwards, DJ and Trujillo, LT, Brain Sci (2021); Holler, Y, et al., CNS Drugs (2018) * Denotes pairwise comparison P < 0.05 Frontal = Fz-Cz; left parietal = Pz-O1; right parietal = PzO2 CFB = change from baseline; Source: Trevena data on file |
|
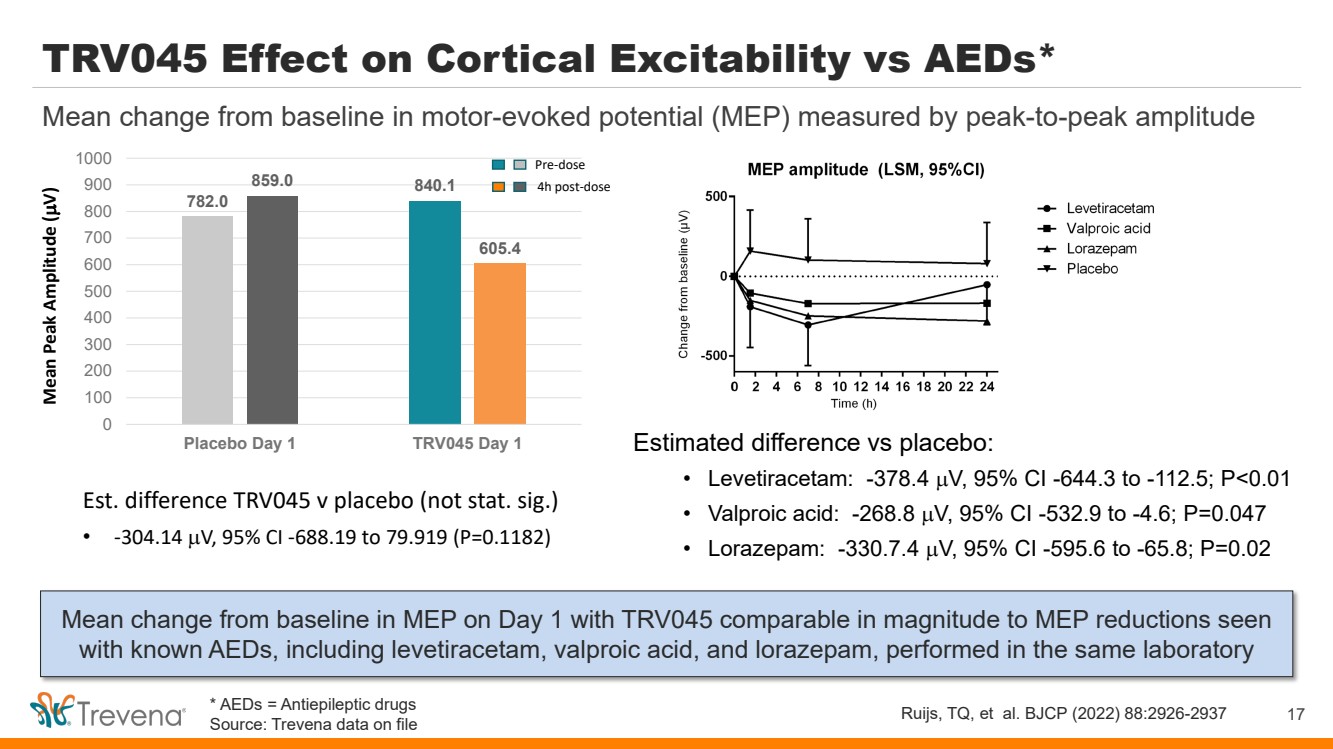
TRV045 Effect on Cortical Excitability vs AEDs* Mean change from baseline in MEP on Day 1 with TRV045 comparable in magnitude to MEP reductions seen with known AEDs, including levetiracetam, valproic acid, and lorazepam, performed in the same laboratory 17 Mean change from baseline in motor-evoked potential (MEP) measured by peak-to-peak amplitude Ruijs, TQ, et al. BJCP (2022) 88:2926-2937 Estimated difference vs placebo: • Levetiracetam: -378.4 µV, 95% CI -644.3 to -112.5; P<0.01 • Valproic acid: -268.8 µV, 95% CI -532.9 to -4.6; P=0.047 • Lorazepam: -330.7.4 µV, 95% CI -595.6 to -65.8; P=0.02 782.0 840.1 859.0 605.4 0 100 200 300 400 500 600 700 800 900 1000 Placebo Day 1 TRV045 Day 1 Mean Peak Amplitude ( µV) Pre-dose 4h post-dose Est. difference TRV045 v placebo (not stat. sig.) • -304.14 µV, 95% CI -688.19 to 79.919 (P=0.1182) * AEDs = Antiepileptic drugs Source: Trevena data on file |
|
Safety and Tolerability Summary • No AEs assessed as probably / definitely related to study drug; no AEs reported as severe; no SAEs - 98% of AEs (102 of 104) in PainCart® study reported as mild - 99% of AEs (79 of 80) in TMS study reported as mild • Screening / follow-up physical exams (including ophthalmologic exams) with no clinically significant findings • Lab results showed no drug-related: Reduction in total lymphocyte count Changes in heart rate or blood pressure Changes in ECG interval measures (no prolongation of PR or QTcF intervals) 18 POC data generally consistent with FIH study |
|
Safety and Tolerability Summary • AEs with incidence of ≥10% for any TRV045 dose shown below (none deemed drug related) • No clinically signficant difference (vs placebo) in any AEs including: Sedation Balance Disorders Attention Disturbances Nausea Dry Mouth Blurred Vision • 19 Generally well tolerated and consistent with FIH study PainCart Study Placebo TRV045 50mg TRV045 150mg TRV045 300mg N (%) Events N (%) Events N (%) Events N (%) Events General Disorders Fatigue 3 (12%) 3 1 (4%) 1 3 (12%) 3 2 (8%) 2 Nervous System Disorders Dizziness Headache Somnolence 2 (8%) 2 (8%) 2 (8%) 2 2 3 0 3 (12%) 2 (8%) 0 3 2 3 (12%) 8 (32%) 5 (20%) 3 9 5 3 (12%) 8 (32%) 8 (32%) 3 9 8 TMS Study Placebo TRV045 250mg N (%) Events N (%) Events General Disorders Fatigue 1 (4%) 3 3 (12%) 5 Nervous System Disorders Headache Somnolence 6 (22%) 4 (15%) 8 3 9 (36%) 3 (12%) 12 4 FIH = First in human |
|
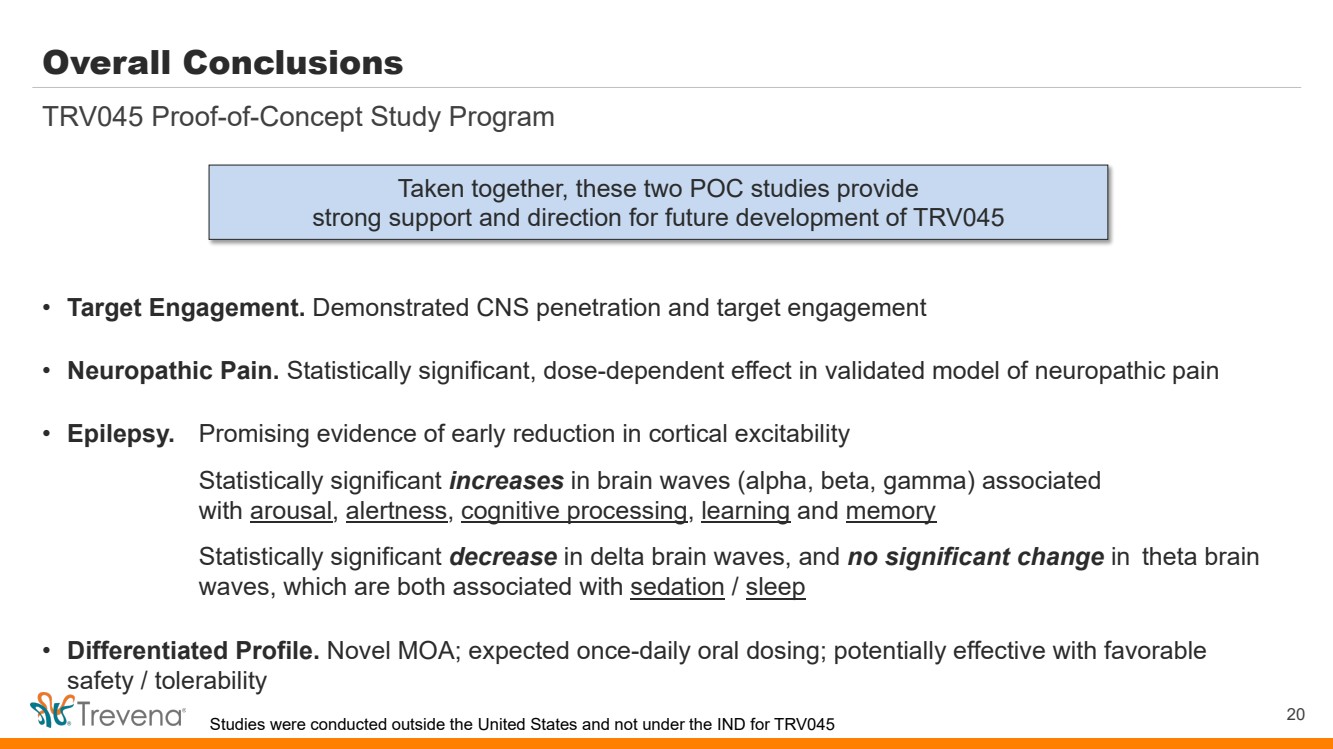
Overall Conclusions • Target Engagement. Demonstrated CNS penetration and target engagement • Neuropathic Pain. Statistically significant, dose-dependent effect in validated model of neuropathic pain • Epilepsy. Promising evidence of early reduction in cortical excitability Statistically significant increases in brain waves (alpha, beta, gamma) associated with arousal, alertness, cognitive processing, learning and memory Statistically significant decrease in delta brain waves, and no significant change in theta brain waves, which are both associated with sedation / sleep • Differentiated Profile. Novel MOA; expected once-daily oral dosing; potentially effective with favorable safety / tolerability TRV045 Proof-of-Concept Study Program Taken together, these two POC studies provide strong support and direction for future development of TRV045 Studies were conducted outside the United States and not under the IND for TRV045 20 |
|
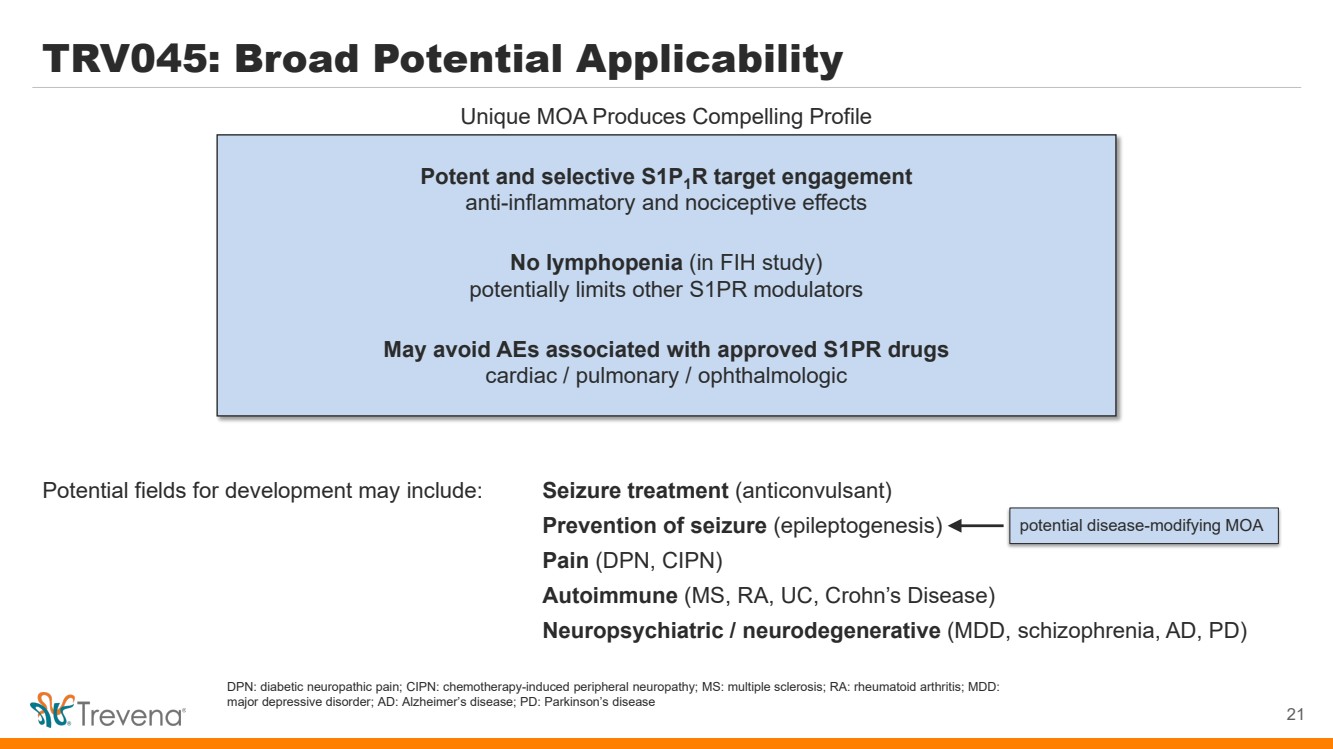
TRV045: Broad Potential Applicability Potential fields for development may include: Seizure treatment (anticonvulsant) Prevention of seizure (epileptogenesis) Pain (DPN, CIPN) Autoimmune (MS, RA, UC, Crohn’s Disease) Neuropsychiatric / neurodegenerative (MDD, schizophrenia, AD, PD) Potent and selective S1P1R target engagement anti-inflammatory and nociceptive effects No lymphopenia (in FIH study) potentially limits other S1PR modulators May avoid AEs associated with approved S1PR drugs cardiac / pulmonary / ophthalmologic 21 Unique MOA Produces Compelling Profile potential disease-modifying MOA DPN: diabetic neuropathic pain; CIPN: chemotherapy-induced peripheral neuropathy; MS: multiple sclerosis; RA: rheumatoid arthritis; MDD: major depressive disorder; AD: Alzheimer’s disease; PD: Parkinson’s disease |
|
TRV045: Innovative Clinical-Stage S1P1R Modulator TRV045: Selective S1PR Modulator Compelling Clinical POC Data1 Differentiated Product Profile Large Addressable Target Indications Novel Family of S1PR Modulators S1PR: Validated target for multiple blockbusters (fingolimod / siponimod / ozanimod / ponesimod) TRV045: Unique profile with no lymphopenia or cardiac / ophthalmologic / pulmonary AEs Statistically significant, dose-dependent effect in validated model of neuropathic pain Statistically significant EEG changes and evidence of early reduction in cortical excitability Novel MOA; expected once daily oral dosing; potentially effective with favorable safety/tolerability Potential for favorable cognitive profile vs current SOC Initial investigation for orphan / non-orphan non-opioid chronic pain and epilepsy Broad potential application in CNS disorders, autoimmune disease and inflammatory disease New chemical entity; potent and selective for subtype 1; developed in-house with strong IP NIH collaboration: Epilepsy Therapy Screening Program & Preclinical Screening Pain Platform 22 SOC = Standard of Care MOA = Mechanism of action 1Studies were conducted outside the United States and not under the IND for TRV045 |
|
TRV045 Prior FIH Phase 1 Study |
|
TRV045 Phase 1 Study – Safety / Tolerability / PK Randomized, double-blinded, placebo-controlled study 3-parts: single dose (n=53), food effect (n=27), multiple dose (n=9) 24 Well Tolerated • Favorable tolerability profile with no SAEs Target Exposure Attractive PK Profile • Calculated free plasma concentrations exceeded targeted efficacy range1 • Half-life consistent with anticipated once-daily dosing Highly Differentiated • No lymphopenia and no reported cardiac / pulmonary / ophthalmologic AEs (AEs commonly associated with currently marketed S1P-targeted compounds) 1 Based on nonclinical measures of in vitro and in vivo PD |
|
TRV045 Nonclinical Data - Epilepsy |
|
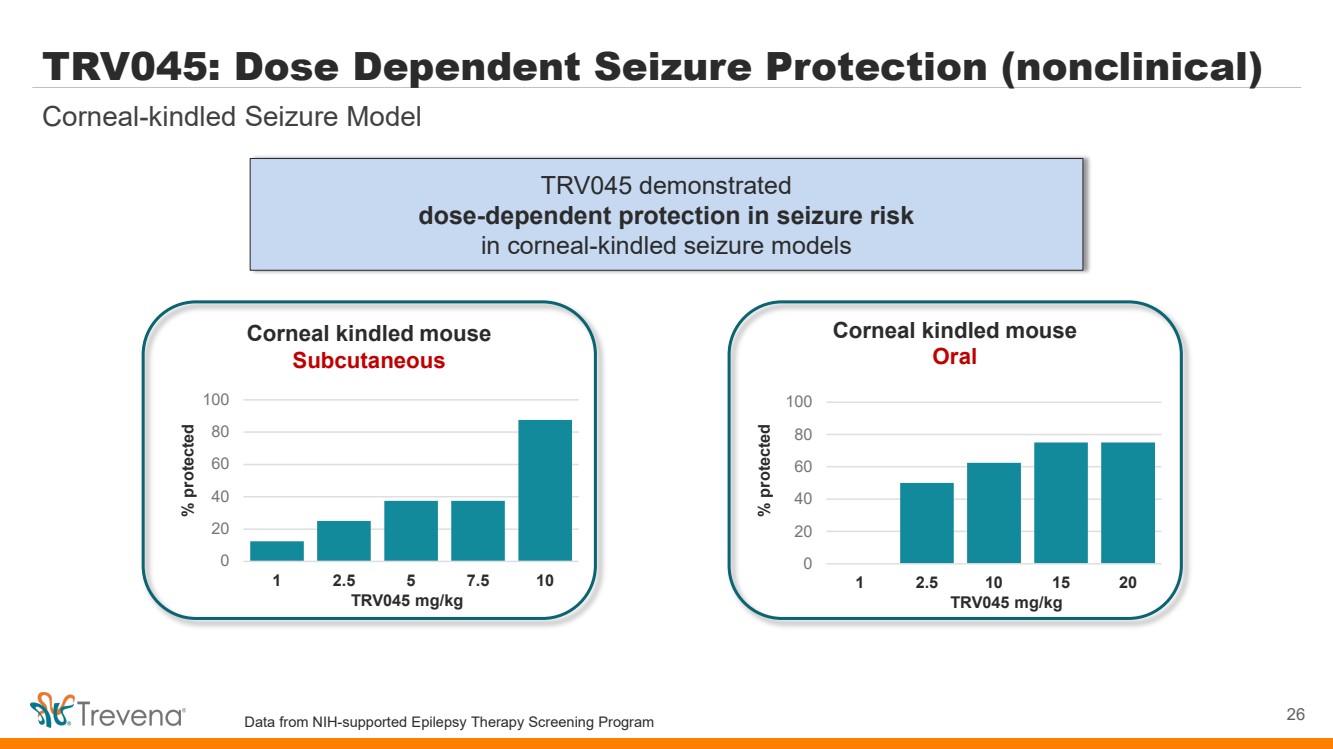
TRV045 demonstrated dose-dependent protection in seizure risk in corneal-kindled seizure models Corneal-kindled Seizure Model TRV045: Dose Dependent Seizure Protection (nonclinical) 26 Corneal kindled mouse Subcutaneous 0 20 40 60 80 100 1 2.5 5 7.5 10 % protected TRV045 mg/kg Corneal kindled mouse Oral 0 20 40 60 80 100 1 2.5 10 15 20 % protected TRV045 mg/kg Data from NIH-supported Epilepsy Therapy Screening Program |
|
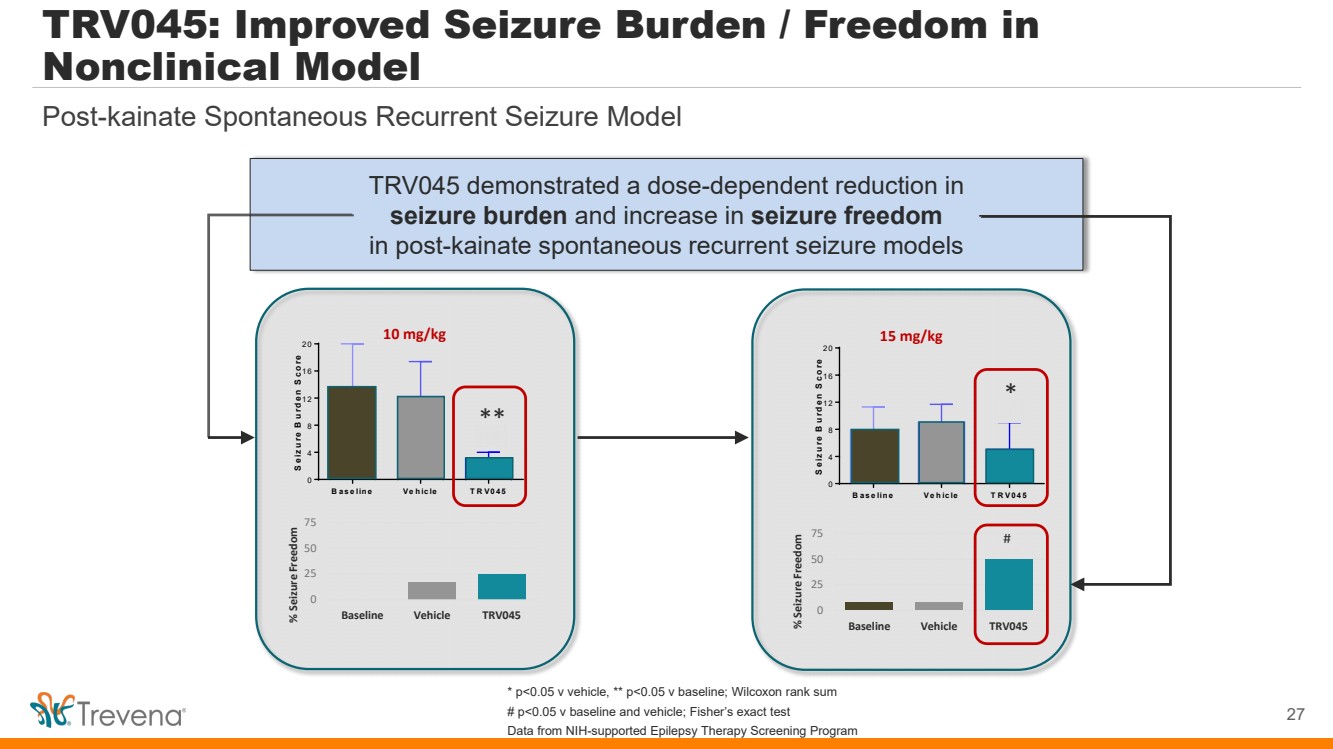
B ase line Ve hicle T RV045 0 4 8 1 2 1 6 2 0 Seizure B urden S core * 15 mg/kg * # 0 25 50 75 % Seizure Freedom Baseline Vehicle TRV045 B ase line Ve hicle T RV045 0 4 8 1 2 1 6 2 0 Seizure B urden S core * 10 mg/kg ** 0 25 50 75 % Seizure Freedom Baseline Vehicle TRV045 TRV045 demonstrated a dose-dependent reduction in seizure burden and increase in seizure freedom in post-kainate spontaneous recurrent seizure models Post-kainate Spontaneous Recurrent Seizure Model TRV045: Improved Seizure Burden / Freedom in Nonclinical Model 27 * p<0.05 v vehicle, ** p<0.05 v baseline; Wilcoxon rank sum # p<0.05 v baseline and vehicle; Fisher’s exact test Data from NIH-supported Epilepsy Therapy Screening Program |
|
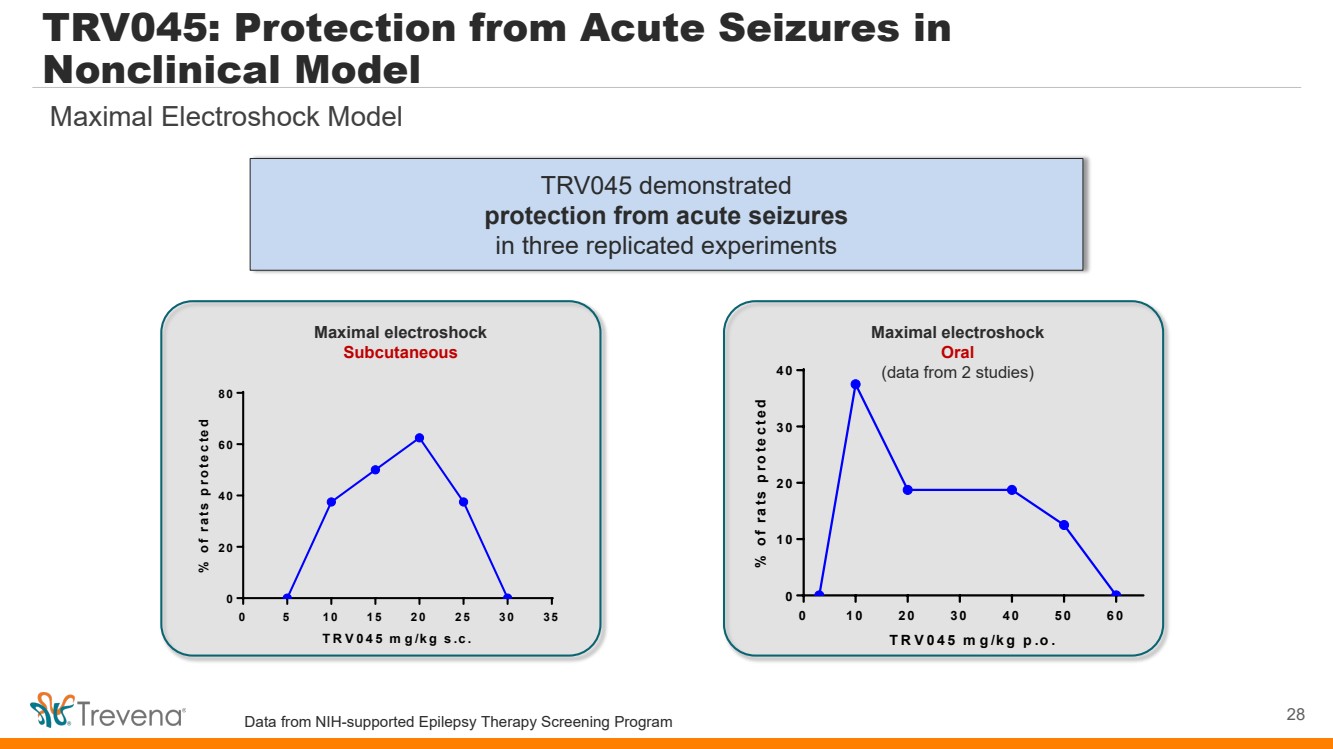
TRV045 demonstrated protection from acute seizures in three replicated experiments TRV045: Protection from Acute Seizures in Nonclinical Model 28 Maximal Electroshock Model 0 5 1 0 1 5 2 0 2 5 3 0 3 5 0 2 0 4 0 6 0 8 0 TR V045 m g/kg s.c. % of rats protected Maximal electroshock Subcutaneous 0 1 0 2 0 3 0 4 0 5 0 6 0 0 1 0 2 0 3 0 4 0 TR V045 m g/kg p.o. % of rats protected Maximal electroshock Oral (data from 2 studies) Data from NIH-supported Epilepsy Therapy Screening Program |
|
TRV045 Nonclinical Data – Non-opioid Pain Indications |
|
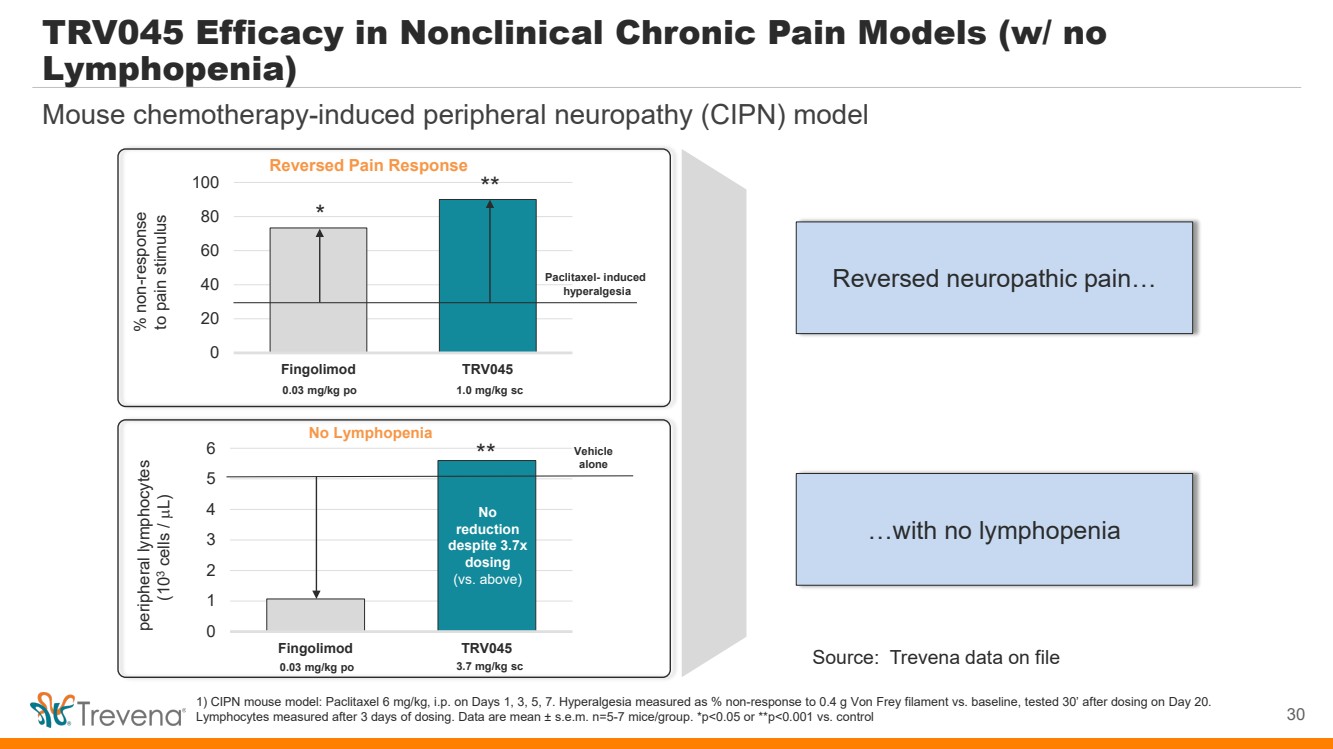
0 1 2 3 4 5 6 Fingolimod TRV045 No Lymphopenia TRV045 Efficacy in Nonclinical Chronic Pain Models (w/ no Lymphopenia) 1) CIPN mouse model: Paclitaxel 6 mg/kg, i.p. on Days 1, 3, 5, 7. Hyperalgesia measured as % non-response to 0.4 g Von Frey filament vs. baseline, tested 30’ after dosing on Day 20. Lymphocytes measured after 3 days of dosing. Data are mean ± s.e.m. n=5-7 mice/group. *p<0.05 or **p<0.001 vs. control peripheral lymphocytes (103 cells / µL) 0.03 mg/kg po 3.7 mg/kg sc Vehicle alone No reduction despite 3.7x dosing (vs. above) ** Reversed Pain Response 0 20 40 60 80 100 Fingolimod TRV045 % non-response to pain stimulus 0.03 mg/kg po 1.0 mg/kg sc Paclitaxel- induced hyperalgesia * ** 30 Mouse chemotherapy-induced peripheral neuropathy (CIPN) model Reversed neuropathic pain… …with no lymphopenia Source: Trevena data on file |
|
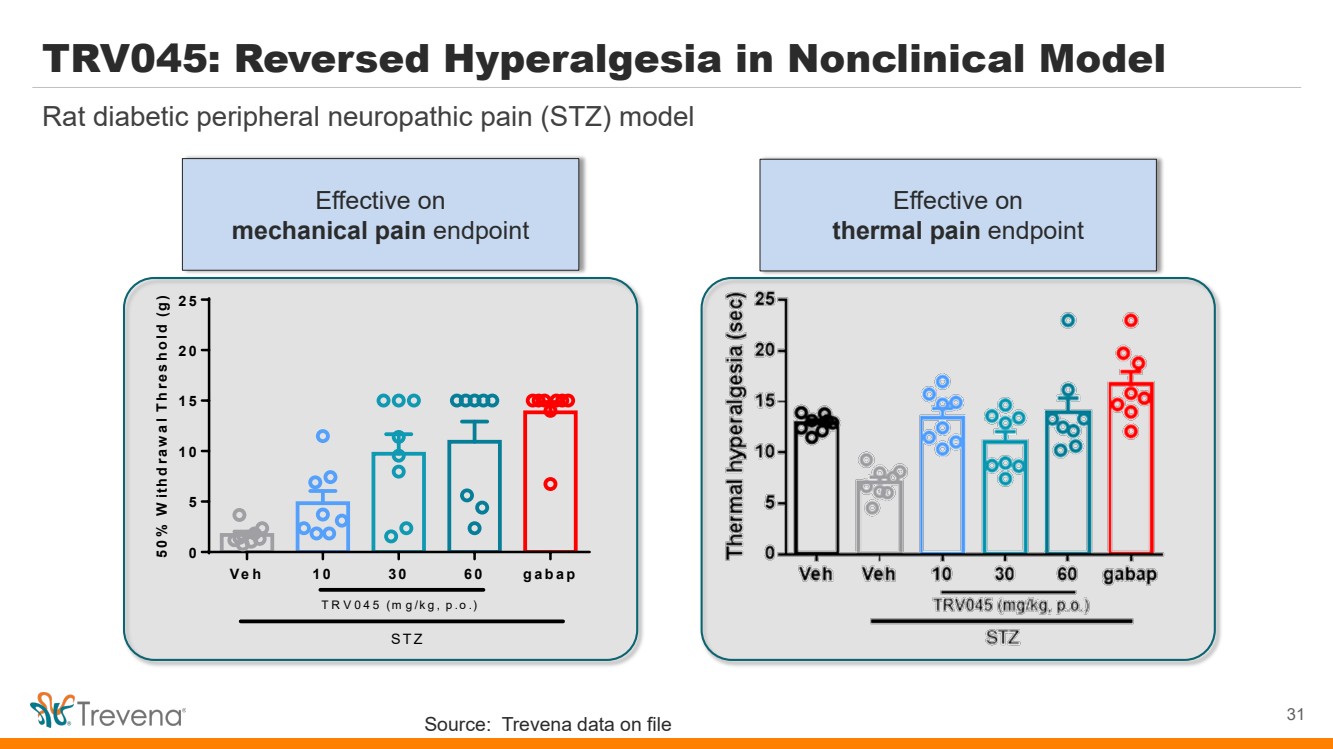
Rat diabetic peripheral neuropathic pain (STZ) model TRV045: Reversed Hyperalgesia in Nonclinical Model 31 Veh 1 0 3 0 6 0 gabap 0 5 1 0 1 5 2 0 2 5 50% W ithdraw al Threshold (g) STZ TR V 045 (m g/kg, p.o.) Effective on thermal pain endpoint Effective on mechanical pain endpoint Source: Trevena data on file |
|
32 IMPORTANT SAFETY INFORMATION |
|
WARNING: ADDICTION, ABUSE, AND MISUSE; LIFE-THREATENING RESPIRATORY DEPRESSION; NEONATAL OPIOID WITHDRAWAL SYNDROME; and RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CENTRAL NERVOUS SYSTEM (CNS) DEPRESSANTS Addiction, Abuse, and Misuse OLINVYK exposes patients and other users to the risks of opioid addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient’s risk before prescribing OLINVYK, and monitor all patients regularly for the development of behaviors or conditions. Life-Threatening Respiratory Depression Serious, life-threatening, or fatal respiratory depression may occur with use of OLINVYK. Monitor for respiratory depression, especially during initiation of OLINVYK or following a dose increase. Neonatal Opioid Withdrawal Syndrome Prolonged use of OLINVYK during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. Risk From Concomitant Use With Benzodiazepines or Other CNS Depressants Concomitant use of opioids with benzodiazepines or other CNS depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing for use in patients for whom alternative treatment options are inadequate; limit dosages and durations to the minimum required; and follow patients for signs and symptoms of respiratory depression and sedation. Limitations of Use Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, reserve OLINVYK for use in patients for whom alternative treatment options [e.g., non-opioid analgesics or opioid combination products]: • Have not been tolerated, or are not expected to be tolerated • Have not provided adequate analgesia, or are not expected to provide adequate analgesia. The cumulative total daily dose should not exceed 27 mg, as total daily doses greater than 27 mg may increase the risk for QTc interval prolongation. CONTRAINDICATIONS OLINVYK is contraindicated in patients with: • Significant respiratory depression • Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment • Known or suspected gastrointestinal obstruction, including paralytic ileus • Known hypersensitivity to oliceridine (e.g., anaphylaxis) WARNINGS AND PRECAUTIONS • OLINVYK contains oliceridine, a Schedule II controlled substance, that exposes users to the risks of addiction, abuse, and misuse. Although the risk of addiction in any individual is unknown, it can occur in patients appropriately prescribed OLINVYK. Assess risk, counsel, and monitor all patients receiving opioids. • Serious, life-threatening respiratory depression has been reported with the use of opioids, even when used as recommended, especially in patients with chronic pulmonary disease, or in elderly, cachectic and debilitated patients. The risk is greatest during initiation of OLINVYK therapy, following a dose increase, or when used with other drugs that depress respiration. Proper dosing of OLINVYK is essential, especially when converting patients from another opioid product to avoid overdose. Management of respiratory depression may include close observation, supportive measures, and use of opioid antagonists, depending on the patient’s clinical status. • Opioids can cause sleep-related breathing disorders including central sleep apnea (CSA) and sleep-related hypoxemia with risk increasing in a dose-dependent fashion. In patients who present with CSA, consider decreasing the dose of opioid using best practices for opioid taper. INDICATIONS AND USAGE OLINVYK is a new chemical entity indicated in adults for the management of acute pain severe enough to require an intravenous opioid analgesic and for whom alternative treatments are inadequate. 33 |
|
WARNINGS AND PRECAUTIONS • Prolonged use of opioids during pregnancy can result in withdrawal in the neonate that may be life-threatening. Observe newborns for signs of neonatal opioid withdrawal syndrome and manage accordingly. Advise pregnant women using OLINVYK for a prolonged period of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. • Profound sedation, respiratory depression, coma, and death may result from the concomitant use of OLINVYK with benzodiazepines or other CNS depressants (e.g., non-benzodiazepine sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids, or alcohol). Because of these risks, reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate, prescribe the lowest effective dose, and minimize the duration. • OLINVYK was shown to have mild QTc interval prolongation in thorough QT studies where patients were dosed up to 27 mg. Total cumulative daily doses exceeding 27 mg per day were not studied and may increase the risk for QTc interval prolongation. Therefore, the cumulative total daily dose of OLINVYK should not exceed 27 mg. • Increased plasma concentrations of OLINVYK may occur in patients with decreased Cytochrome P450 (CYP) 2D6 function or normal metabolizers taking moderate or strong CYP2D6 inhibitors; also in patients taking a moderate or strong CYP3A4 inhibitor, in patients with decreased CYP2D6 function who are also receiving a moderate or strong CYP3A4 inhibitor, or with discontinuation of a CYP3A4 inducer. These patients may require less frequent dosing and should be closely monitored for respiratory depression and sedation at frequent intervals. Concomitant use of OLINVYK with CYP3A4 inducers or discontinuation of a moderate or strong CYP3A4 inhibitor can lower the expected concentration, which may decrease efficacy, and may require supplemental doses. • Cases of adrenal insufficiency have been reported with opioid use (usually greater than one month). Presentation and symptoms may be nonspecific and include nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. If confirmed, treat with physiologic replacement doses of corticosteroids and wean patient from the opioid. • OLINVYK may cause severe hypotension, including orthostatic hypotension and syncope in ambulatory patients. • There is increased risk in patients whose ability to maintain blood pressure has already been compromised by a reduced blood volume or concurrent administration of certain CNS depressant drugs (e.g., phenothiazines or general anesthetics). Monitor these patients for signs of hypotension. In patients with circulatory shock, avoid the use of OLINVYK as it may cause vasodilation that can further reduce cardiac output and blood pressure. • Avoid the use of OLINVYK in patients with impaired consciousness or coma. OLINVYK should be used with caution in patients who may be susceptible to the intracranial effects of CO2 retention, such as those with evidence of increased intracranial pressure or brain tumors, as a reduction in respiratory drive and the resultant CO2 retention can further increase intracranial pressure. Monitor such patients for signs of sedation and respiratory depression, particularly when initiating therapy. • As with all opioids, OLINVYK may cause spasm of the sphincter of Oddi, and may cause increases in serum amylase. Monitor patients with biliary tract disease, including acute pancreatitis, for worsening symptoms. • There is increased risk in patients whose ability to maintain blood pressure has already been compromised by a reduced blood volume or concurrent administration of certain CNS depressant drugs (e.g., phenothiazines or general anesthetics). Monitor these patients for signs of hypotension. In patients with circulatory shock, avoid the use of OLINVYK as it may cause vasodilation that can further reduce cardiac output and blood pressure. • Avoid the use of OLINVYK in patients with impaired consciousness or coma. OLINVYK should be used with caution in patients who may be susceptible to the intracranial effects of CO2 retention, such as those with evidence of increased intracranial pressure or brain tumors, as a reduction in respiratory drive and the resultant CO2 retention can further increase intracranial pressure. Monitor such patients for signs of sedation and respiratory depression, particularly when initiating therapy. • As with all opioids, OLINVYK may cause spasm of the sphincter of Oddi, and may cause increases in serum amylase. Monitor patients with biliary tract disease, including acute pancreatitis, for worsening symptoms. • OLINVYK may increase the frequency of seizures in patients with seizure disorders and may increase the risk of seizures in vulnerable patients. Monitor patients with a history of seizure disorders for worsened seizure control. • Do not abruptly discontinue OLINVYK in a patient physically dependent on opioids. Gradually taper the dosage to avoid a withdrawal syndrome and return of pain. Avoid the use of mixed agonist/antagonist (e.g., pentazocine, nalbuphine, and butorphanol) or partial agonist (e.g., buprenorphine) analgesics in patients who are receiving OLINVYK, as they may reduce the analgesic effect and/or precipitate withdrawal symptoms. • OLINVYK may impair the mental or physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery. • Although self-administration of opioids by patient-controlled analgesia (PCA) may allow each patient to individually titrate to an acceptable level of analgesia, PCA administration has resulted in adverse outcomes and episodes of respiratory depression. Health care providers and family members monitoring patients receiving PCA analgesia should be instructed in the need for appropriate monitoring for excessive sedation, respiratory depression, or other adverse effects of opioid medications. ADVERSE REACTIONS Adverse reactions are described in greater detail in the Prescribing Information. The most common (incidence ≥10%) adverse reactions in Phase 3 controlled clinical trials were nausea, vomiting, dizziness, headache, constipation, pruritus, and hypoxia. PLEASE see www.OLNVYK.com for full prescribing information including BOXED warning and important safety information 34 |